How to manage blood pressure well behind the dispute over diagnostic criteria of hypertension?
Original Shanghai Xinhua Hospital Shanghai Xinhua Hospital
On November 15th, National Health Commission announced that the diagnostic criteria for hypertension in adults have not been adjusted at present. Regarding the diagnostic criteria of hypertension, the publicity and education points, prevention and treatment guidelines and clinical pathways issued by the national health administrative department in 2005, 2010 and 2017 are all clear: the diagnostic criteria of adult hypertension are that the blood pressure exceeds 140/90mmHg for three times on the same day.
Previously, the authoritative guide-Clinical Practice Guide of Hypertension in China, which was jointly formulated by the National Cardiovascular Center, the Chinese Medical Doctor Association and the Cardiovascular Branch of the Chinese Medical Association, was officially promulgated on November 13th. The biggest highlight of the new guidelines is to lower the diagnostic criteria of hypertension to ≥130/80 mmHg. As a result, the debate on the diagnostic criteria of hypertension has been triggered.

Question 1: Why is there a debate about the diagnostic criteria of hypertension?
The diagnostic criteria of hypertension are actually changing.
In 1977, the first diagnostic criteria for hypertension in the world were systolic blood pressure ≥160mmHg and/or diastolic blood pressure ≥ 95 mmHg;
By 1997, the diagnostic criteria of hypertension were lowered to systolic blood pressure ≥140mmHg and/or diastolic blood pressure ≥ 90 mmHg;
In recent years, more and more research data show that among adults aged 18 and above, the incidence and mortality of cardiovascular diseases in people with systolic blood pressure of 130~139 mmHg and/or diastolic blood pressure of 80~89 mmHg are still extremely high. Therefore, in 2017, the American College of Cardiology, ACC) and American Heart Association (AHA) further reduced the diagnostic criteria of hypertension to systolic blood pressure ≥130 mmHg and/or diastolic blood pressure ≥80 for the first time. However, considering that the number of patients with hypertension will increase significantly, and it will bring corresponding medical expenses and economic burdens, the diagnostic criteria of 140/90mmHg are maintained in the 2018 edition of the European Guidelines, the International Hypertension Practice Guidelines of the International Hypertension Society (ISH) in 2020, and the Adult Hypertension Drug Treatment Guidelines of the World Health Organization (WHO) in 2021, as well as the national hypertension guidelines except the United States.
With the publication of many clinical research results in China, researchers found that among adults aged 18 and above in China, the proportion of people with systolic blood pressure of 130~139 mmHg and/or diastolic blood pressure of 80~89 mmHg was 23.2%, and the estimated total number was nearly 243 million. In the past 15 years, 65% of these people progressed to blood pressure of ≥ 140/90 mmHg [3,4]. Based on these evidences, the new guidelines
Therefore, whether the diagnostic standard of systolic blood pressure of hypertension is ≥130 mmHg or ≥140 mmHg has always been the focus of clinical research, and we need more research data from domestic population to support it.
Question 2: Hypertension has no symptoms. Is it harmful?
Hypertension is the most common high-risk factor leading to the death of people, also known as the "silent killer". If blood pressure is not controlled, the risk of death of patients within 10 years is obviously increased. The main harm of hypertension is the overload of the heart and the progression of systemic atherosclerosis, and the higher the blood pressure, the faster the progress, and all organs covered by arteries will be affected, and the most common is the damage to the heart, kidneys and intracranial blood vessels, which usually leads to "big heart, small kidney and stroke".

Question 3: How to measure blood pressure correctly?
When adults measure blood pressure, they can use the upper arm electronic sphygmomanometer verified by the standardized scheme on the market at present to measure blood pressure.
The specific measurement method is:
1. Take a quiet rest for 3~5 minutes before measuring blood pressure. When measuring, sit in a chair with a backrest, put your feet flat on the ground and don’t cross your legs. The upper arm is flat on the desktop, and the center of the cuff of the sphygmomanometer is kept at the same level as the heart.
2. Choose a suitable cuff for blood pressure measurement, and wrist electronic sphygmomanometer can be selected if the upper arm circumference is more than 42 cm.
3. The upper arm for measuring blood pressure should be fully exposed or only covered with a single layer of clothing (do not wear sleeves), and the lower edge of the cuff should be placed 2~3 cm above the elbow socket.
4. Get at least two blood pressure readings every time you measure blood pressure, with an interval of 1~2 minutes, and take the average of the two readings; If the difference between the first and second blood pressure readings is greater than 10 mmHg, it is recommended to measure it for the third time and take the average of the last two blood pressure readings. When measuring blood pressure for the first time, the blood pressure of both upper arms should be measured, whichever side is higher.
5. It is recommended that patients with atrial fibrillation (AF) use electronic sphygmomanometer to measure their blood pressure, and at least three blood pressure readings should be obtained for each measurement, and the average of the three blood pressure readings should be taken.
In the process of diagnosis and management of hypertension, hospital clinic blood pressure measurement, family blood pressure monitoring and 24-hour ambulatory blood pressure monitoring can all be used as effective measurement methods in diagnosis and management of hypertension. For the diagnosis of hypertension, 24-hour ambulatory blood pressure monitoring is preferred if conditions permit; For hypertension management, it is suggested that home blood pressure monitoring should be the first choice.
Blood pressure monitoring at home is also very particular.
These key points of blood pressure monitoring must be written down!
1. It is recommended to measure blood pressure once every morning and once every night;
2. Avoid strenuous exercise, drinking, drinking caffeinated drinks and smoking 30 minutes before measuring blood pressure;
3. It is recommended to measure blood pressure before taking medicine, before breakfast and after emptying the bladder in the morning;
4. It is recommended to measure blood pressure before dinner at night, and it is recommended to measure it within 1 hour before going to bed when conditions do not permit;
5. For patients who are newly diagnosed or whose blood pressure is not controlled, it is recommended to monitor their blood pressure at home for at least 3 consecutive days every week, and record the monitoring results, which is an important basis for doctors to diagnose and adjust the antihypertensive treatment plan for you.
Question 4: Do people with systolic blood pressure between 130 and 139 mmHg need medication?
① For patients with systolic blood pressure of 130~139 mmHg and/or DBP of 80 ~ 89 mmHg, lifestyle intervention can be carried out for 3~6 months if there are only 2 cardiovascular risk factors after evaluation by professional doctors.
② Systolic blood pressure of 130~139 mmHg and/or diastolic blood pressure of 80~89 mmHg with clinical complications, or patients with target organ damage or with more than 3 cardiovascular risk factors after evaluation by professional doctors, it is suggested to start antihypertensive drug therapy.
Question 5: What are the cardiovascular risk factors?
According to the guidelines, cardiovascular risk factors mainly include:
Age (male ≥45, female ≥55);
Smoking or passive smoking;
High density lipoprotein cholesterol < 1.04 mmol/L (40 mg/DL);
Low density lipoprotein cholesterol ≥ 3.4 mmol/L (130 mg/DL);
Abnormal fasting blood glucose (6.1 ~ 6.9 mmol/L);
Obesity (body mass index ≥28.0 kg/m2).
The new standards determined in the new edition of the guidelines are more aimed at people with borderline hypertension, and its main purpose is to improve the attention of these people to health conditions. Diagnosing hypertension doesn’t mean taking medicine immediately. In the absence of other risk factors, patients with blood pressure at the critical value usually only need to adjust their daily ways, such as quitting smoking and drinking and exercising properly, to improve their physical condition.
Question 6: What are the life intervention measures for patients with hypertension?
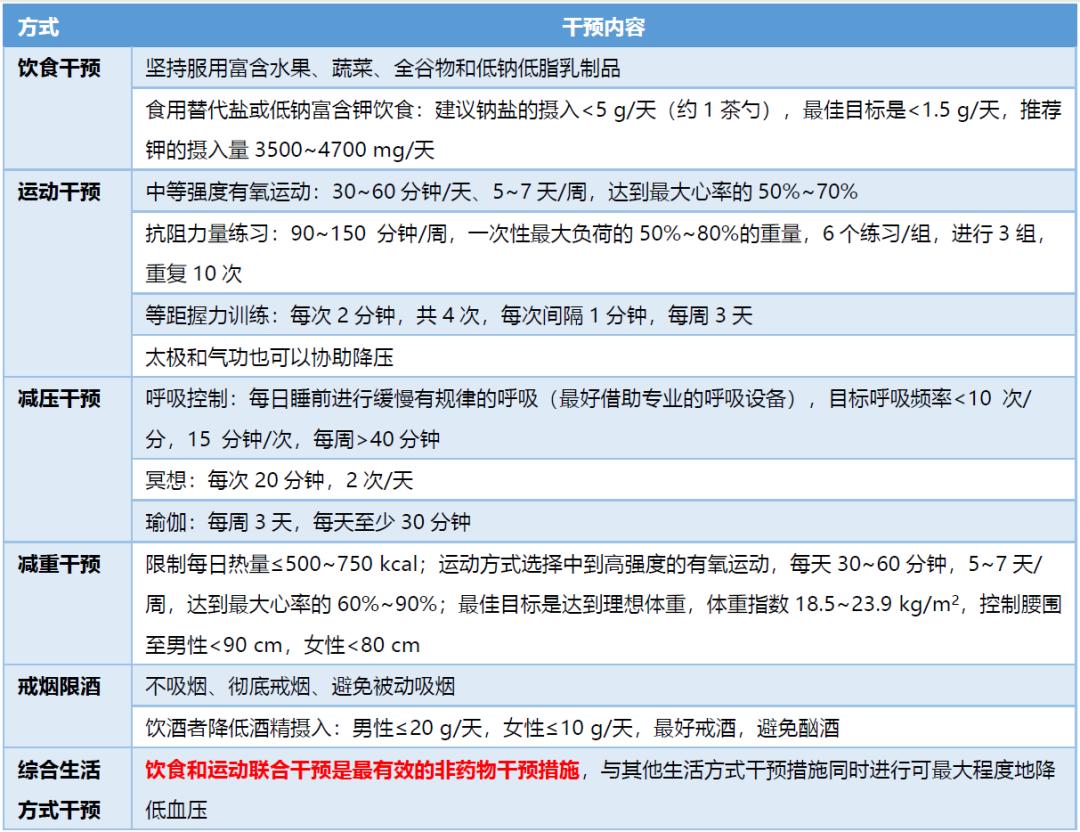
Lifestyle intervention is the cornerstone of hypertension treatment. It is suggested that all patients with hypertension should have lifestyle intervention, including diet intervention, exercise intervention, decompression intervention, weight loss intervention, smoking cessation and alcohol restriction and comprehensive lifestyle intervention.
Table 1: Life Intervention Measures for Hypertension Patients Recommended by Guidelines
Question 6: What are the drugs for treating hypertension and what are their side effects?
At present, there are many kinds of antihypertensive drugs in clinic. Commonly used antihypertensive drugs include diuretics, beta blockers, calcium channel blockers and angiotensin converting enzyme inhibitors.
These antihypertensive drugs can relax blood vessels and reduce blood volume through different ways, and finally achieve the purpose of lowering blood pressure.
Many people are worried that taking antihypertensive drugs will affect their liver and kidneys. In fact, it is not necessary. Routine physical examination items include biochemical indicators such as liver and kidney function, and we can clearly see whether drugs have an impact on them. However, after decades of large-scale drug use in the global population, it is found that serious side effects are extremely rare.
Table 2: Representative drugs and side effects of antihypertensive drugs commonly used in clinic at present

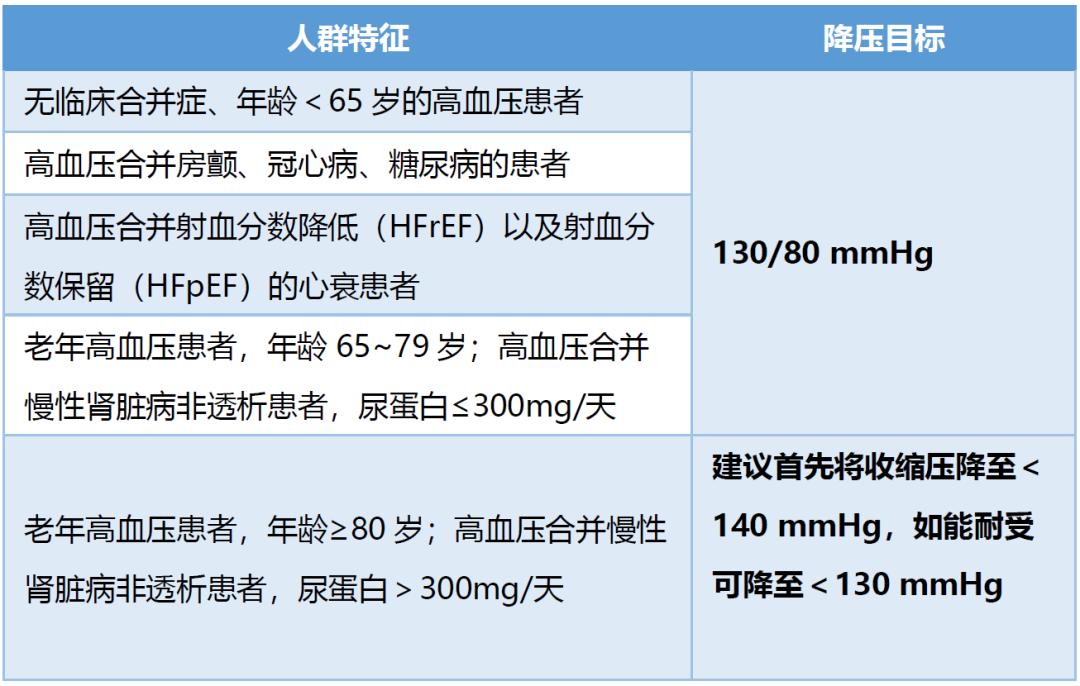
Question 7: What is the target value of antihypertensive treatment for different hypertensive people?
A large number of clinical research results have confirmed that the risk of cerebral infarction, myocardial infarction, heart failure and other diseases will decrease by 10% for every 5mmHg decrease in systolic blood pressure, and controlling blood pressure has great benefits.
However, it should also be noted that antihypertensive drugs may also lead to adverse events such as hypotension, syncope, electrolyte abnormality and acute kidney injury or failure. Therefore, the antihypertensive plan must follow the advice of professional doctors and should not be adjusted by itself.
Table 3: Target value of antihypertensive treatment for hypertensive patients recommended by guidelines
Question 8: Can I stop taking medicine if I have no symptoms or my blood pressure drops to normal?
The main harm of hypertension is not the symptoms it causes, but the chronic damage to the heart, brain, kidney and other organs unconsciously. When these damages become more and more serious, various complications will occur that seriously affect the quality of life and even endanger life.
More than 95% of hypertension belongs to "essential hypertension", the cause of which is unknown. It can only be controlled and cannot be cured. Most people need to take medicine for life.
The "normal" blood pressure after taking medicine is only a state under the action of drugs, and the action time of drugs is limited. Once the drugs are stopped, the drug effect will gradually disappear and blood pressure will rise again.
Therefore, even if your blood pressure is temporarily controlled, you should not stop taking drugs without authorization. If hypotension occurs, or blood pressure is always within the normal range, you can consult a specialist and gradually reduce the types and dosage of drugs under the guidance.
Question 9: Is there any way to reduce hypertension through surgical treatment?
At present, the current control rate of hypertension is less than 20%. In addition to the low awareness rate of hypertension, there are also problems of drug use and patient compliance.
In the past 20 years, renal sympathectomy through minimally invasive intervention came into being, and has achieved good clinical treatment results. In patients with refractory hypertension, renal sympathectomy can still significantly reduce blood pressure after 36 months. Renal sympathectomy can be used as a strategy to reduce blood pressure in patients with refractory hypertension who can not tolerate antihypertensive drugs and whose clinical characteristics are consistent with hypersympathetic function.
Pay attention to your blood pressure health from now on!
Early treatment will benefit early.
Cardiovascular and cerebrovascular diseases are far away from you!
References:
[1]. National Cardiovascular Center, Chinese Medical Doctor Association, Hypertension Professional Committee of Chinese Medical Doctor Association, Cardiovascular Branch of Chinese Medical Association, Hypertension Professional Committee of Cross-Strait Medical and Health Exchange Association. China Hypertension Clinical Practice Guide. chinese journal of cardiology, 2022, Vol.50, No.11.
[2]. Sun Yingxian. Changes and enlightenment of diagnostic criteria for hypertension. chinese journal of practical internal medicine, 2019,39 (1): 57. DOI: 10.19538.
[3]. Qi Y, Han X, Zhao D, et al. Long‑term cardiovascular risk associated with stage 1 hypertension defined by the 2017 ACC/AHA hypertension guideline. J Am Coll Cardiol, 2018, 72(11): 1201‑1210. DOI: 10.1016.
[4]. Luo D, Cheng Y, Zhang H, et al. Association between high blood pressure and long-term cardiovascular events in young adults: systematic review and meta‑analysis. BMJ, 2020, 370:m3222.
Author’s introduction

